Sexual activity is often discussed mainly in terms of intimacy, connection, and pleasure, but it also has important effects on other body systems, including the urinary system.
During intercourse, increased movement, warmth, and moisture create conditions that can allow bacteria from surrounding skin areas to move closer to the urethra, the small tube that carries urine out of the body. When this happens, bacteria may enter the urinary tract and, in some cases, lead to infection.
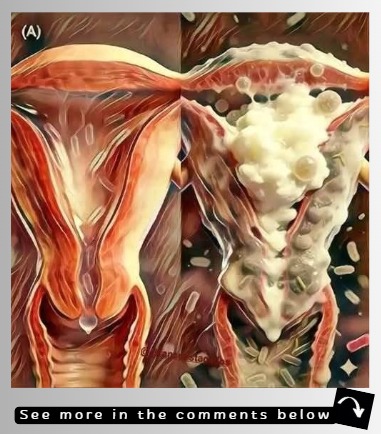
This risk is generally higher in women because of basic anatomy. The female urethra is shorter and located closer to both the vaginal and anal openings, making it easier for bacteria to travel into the bladder.

Men have a longer urethra, which offers more natural protection, but urinary issues can still occur, especially when combined with dehydration, prolonged sexual activity, or inadequate hygiene. No one is completely immune, and both sexes benefit from understanding how sexual habits affect urinary health.
The urinary system relies heavily on regular urine flow to protect itself. Urine helps flush out bacteria before they have time to attach to the lining of the urethra or bladder.
When urination is delayed after sexual activity, bacteria are given more time to settle and multiply. This increases the likelihood of infection, particularly in people who are already prone to urinary tract infections (UTIs).
UTIs often develop gradually, which can make their cause difficult to pinpoint. Symptoms may not appear immediately after sexual activity, leading people to overlook the connection.
Several factors can weaken the body’s ability to flush bacteria effectively, including low fluid intake, holding urine for long periods, physical fatigue, hormonal changes, and a weakened immune system. Stress and lack of sleep can also play a role by reducing the body’s natural defenses.
One common condition linked to sexual activity is postcoital cystitis, a bladder infection that occurs after intercourse. It is most often caused by Escherichia coli (E. coli), a bacterium that normally lives in the digestive tract. During sexual activity, this bacterium can be transferred to the urethra and move upward into the bladder. Symptoms of postcoital cystitis may include a burning sensation during urination, frequent urges to urinate even when the bladder is not full, pelvic pressure or discomfort, and cloudy or strong-smelling urine.
For individuals who experience recurring urinary infections, the impact can go beyond physical discomfort. Repeated symptoms can interfere with daily activities, work, sleep, and emotional well-being. Some people may develop anxiety around intimacy, worrying that sexual activity will lead to pain or infection. It is important to understand that these infections are common and do not reflect poor cleanliness or personal failure. They are often the result of anatomy, biology, and simple mechanical factors.
One of the easiest and most effective preventive measures is urinating shortly after intercourse. This simple habit helps flush bacteria out of the urethra before they have time to multiply or move into the bladder. It supports the body’s natural protective system and requires no medication, special products, or expense. While it may not prevent every infection, it significantly reduces risk for many people.
Staying well hydrated is another key factor. Drinking enough water throughout the day increases urine production, which helps continuously cleanse the urinary tract. Gentle hygiene practices are also important. Washing the genital area with mild, unscented products and avoiding harsh soaps or douches helps maintain a healthy balance of natural bacteria. Wearing breathable, loose-fitting underwear and avoiding prolonged dampness further reduce bacterial growth.
Adequate lubrication during intercourse can also help, as dryness and friction may irritate the urethral opening, making it easier for bacteria to enter. Avoiding unnecessary chemical products, spermicides, or heavily fragranced items can protect sensitive tissues.
With greater awareness and a few simple habits, sexual intimacy can remain both comfortable and healthy. Understanding how sexual activity influences urinary health empowers individuals to take preventive steps, reduce discomfort, and support long-term reproductive and overall physical well-being safely and confidently.